An Introduction to Fertility Treatments: From Ovulation Monitoring to IUI
A comprehensive guide to understanding the foundational fertility treatments available at our clinic, designed to help you on your journey to parenthood.

For many couples, the journey to parenthood is an exciting yet complex path, often involving unexpected detours. If you have been trying to conceive for a year (or six months if you are over 35) without success, you are not alone. Infertility is a common medical challenge, affecting millions of people worldwide. While the path can feel overwhelming, it is essential to remember that modern medicine offers a wide array of highly effective fertility treatments designed to help you achieve your dream.
At Blossom Women’s Clinic, we believe in a tiered approach to fertility care, starting with the least invasive methods and gradually moving to more complex ones as needed. This comprehensive guide will introduce you to the foundational treatments we offer, guiding you through the critical initial steps: from basic ovulation monitoring and medication to the popular intermediate treatment, Intrauterine Insemination (IUI).
1 in 8
Couples Experience Fertility Challenges
85%
Success Rate with Proper Treatment
10M+
Babies Born via Fertility Treatments
Understanding the Initial Assessment and Diagnosis
Before starting any treatment, a thorough investigation is paramount. This initial stage involves diagnostic testing for both partners to pinpoint the cause of infertility, which could be related to ovulatory dysfunction, blocked fallopian tubes, male factor issues, or unexplained infertility (where no clear cause is found). A definitive diagnosis allows your physician to tailor a treatment plan with the highest possible chance of success.

Common initial tests include:
- Hormone Blood Tests (Female): To check baseline levels of key reproductive hormones like Follicle-Stimulating Hormone (FSH), Luteinizing Hormone (LH), Estradiol (Estrogen), Prolactin, and Thyroid hormones (TSH). These results help diagnose ovulatory disorders or pituitary gland issues that affect the cycle.
- Ovarian Reserve Testing (Female): Often done using an Anti-Müllerian Hormone (AMH) blood test to estimate the remaining pool of eggs and provides insight into the ovary’s response potential to fertility medications.
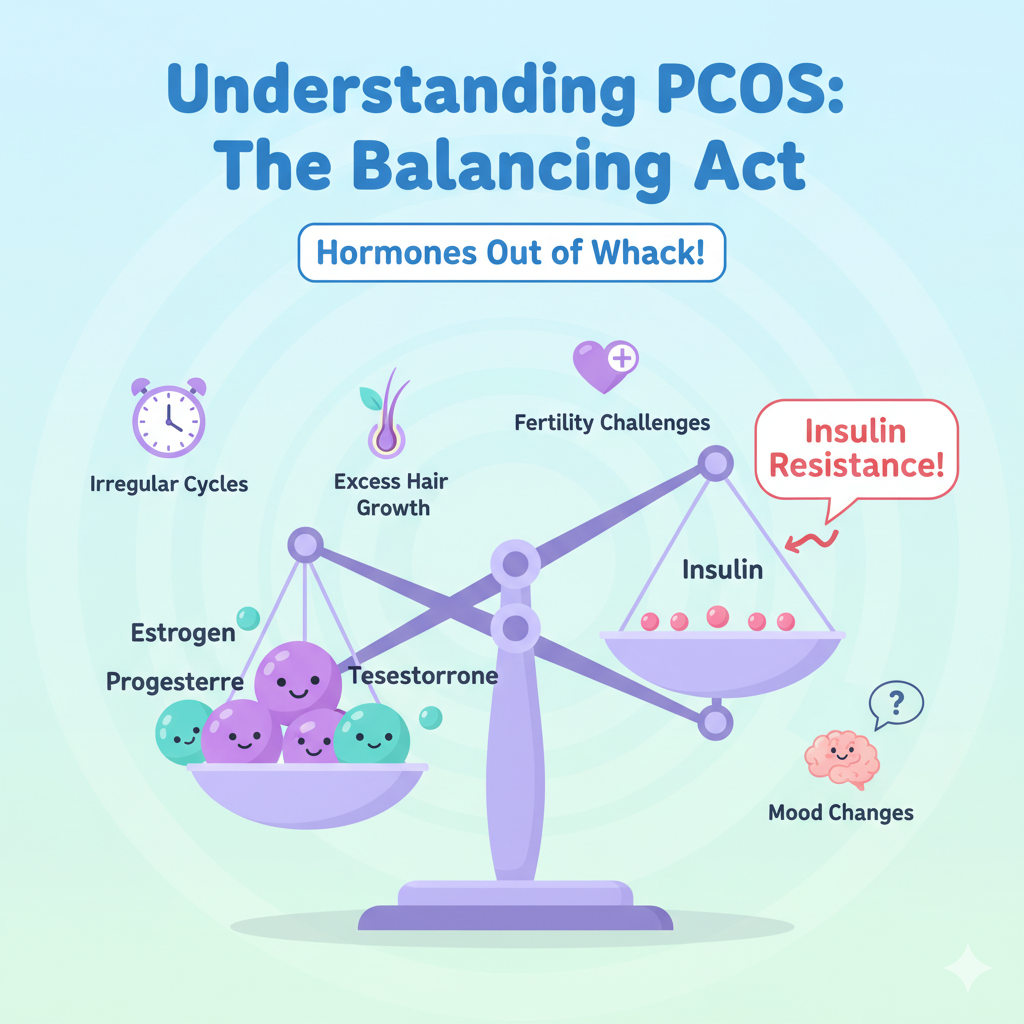
- Imaging (Female): A routine transvaginal ultrasound is performed to check the uterus and ovaries for structural issues like uterine fibroids, endometrial polyps, ovarian cysts, or signs suggestive of Polycystic Ovary Syndrome (PCOS).
- Semen Analysis (Male): This fundamental test evaluates the male partner’s sperm for count (concentration), motility (the percentage of moving sperm), and morphology (the percentage of normally-shaped sperm).
- Hysterosalpingogram (HSG) (Female): This specialized X-ray procedure involves injecting a dye through the cervix into the uterus. It is crucial for checking if the fallopian tubes are open (patent) and if the uterine cavity is normal.
Important: Once a diagnosis is established, we can tailor a treatment plan, which often begins with the most fundamental step: ensuring accurate timing of conception.
Step 1: The Foundation – Ovulation Monitoring and Induction
The simplest and most crucial step in any fertility journey is ensuring that a healthy egg is being released regularly and that intercourse is timed perfectly. For women with irregular cycles or a confirmed ovulatory disorder (like PCOS), this step alone can significantly increase the chances of conception.
What is Ovulation Monitoring?
Ovulation monitoring is the process of tracking the reproductive cycle to precisely identify when an egg is released from the ovary. This process confirms ovulation is occurring and provides the optimal 6-day window, including the day of ovulation and the five preceding days, for conception.

Methods of Ovulation Monitoring:
Basal Body Temperature (BBT) Charting
The Principle: After ovulation, the hormone progesterone causes a slight rise (typically 0.5 to 1.0 degree Fahrenheit) in the woman’s resting body temperature.
Limitation: While useful for confirming that ovulation has already occurred, it is less effective for timing intercourse in the current cycle.
Ovulation Predictor Kits (OPKs)
The Principle: These over-the-counter kits detect the surge of Luteinizing Hormone (LH) in the urine, which happens 24 to 36 hours before the egg is released.
Efficacy: A positive result signals the best time for intercourse over the next two days and is a highly effective at-home method for natural cycles.
Clinical Monitoring (Ultrasound and Bloodwork)
The Principle: This is the most accurate method, performed under medical supervision. It tracks the physical development of the egg follicle in real-time.
The Process: Transvaginal ultrasounds are performed every few days starting early in the cycle to measure the size of the dominant follicle. Blood tests check for rising Estradiol levels and the LH surge.
Ovulation Induction (Medication)
If the initial assessment confirms that ovulation is irregular or absent, the next step is often Ovulation Induction (OI) using oral medications. These drugs work by encouraging the ovaries to produce and release one or more eggs.
- Clomiphene Citrate (Clomid): A selective estrogen receptor modulator (SERM) that tricks the body into thinking estrogen levels are low. This prompts the pituitary gland to release more FSH and LH, stimulating the growth of ovarian follicles.
- Letrozole (Femara): An aromatase inhibitor that temporarily reduces estrogen production. This also stimulates the pituitary gland to release more FSH. It is often preferred for women with PCOS because it typically does not negatively affect the uterine lining and is associated with a lower risk of multiple births compared to Clomid.
Clinical Monitoring is Essential: Once medication is used, clinical monitoring (ultrasound) becomes critical to prevent the risks associated with Ovarian Hyperstimulation Syndrome (OHSS) and to accurately time any subsequent procedure.
Step 2: Intrauterine Insemination (IUI) – The Next Step in Targeted Treatment
For many couples who have not conceived after several cycles of timed intercourse and ovulation induction medication, or for those with specific diagnoses, the next logical and slightly more advanced step is Intrauterine Insemination (IUI), sometimes referred to as artificial insemination.
What is IUI?
IUI is a simple, non-surgical office procedure designed to dramatically increase the concentration of healthy, highly motile sperm that reach the fallopian tubes, thereby significantly improving the chances of fertilization.
It is typically recommended for couples dealing with:
- Mild Male Factor Infertility: Cases with a slightly low sperm count or reduced motility that still meet a minimum threshold after washing.
- Unexplained Infertility: When diagnostic tests for both partners are normal, IUI provides a ‘boost’ to the process.
- Cervical Factor Infertility: The procedure bypasses the cervix, which may contain thick mucus hostile to sperm.
- Use of Donor Sperm: IUI is the primary method for single women or same-sex couples using frozen, quarantined donor sperm.
The IUI Procedure: A Detailed Breakdown
The IUI cycle is typically synchronized with the woman’s medicated cycle (using Clomid, Letrozole, or sometimes injectable hormones), and involves several distinct steps:
1.Ovarian Stimulation and Monitoring
The woman takes fertility drugs starting early in her cycle. The progress of the developing follicles is carefully tracked using transvaginal ultrasounds and blood tests every few days to ensure the development of one to two mature egg follicles.
2.The Trigger Shot
When the lead follicle(s) reach the optimal size (typically 18-20mm), a single injection of human Chorionic Gonadotropin (hCG), often called the “trigger shot,” is administered. This hormone mimics the natural LH surge and causes the final maturation and release of the egg(s) approximately 36 hours later.
3.Sperm Preparation (Washing)
This is a critical, high-tech step performed in the lab on the day of the IUI. The semen sample undergoes a process called sperm washing or preparation. This process isolates the most motile, healthy sperm from the seminal fluid and removes non-motile sperm, dead cells, and chemicals that can cause cramping.
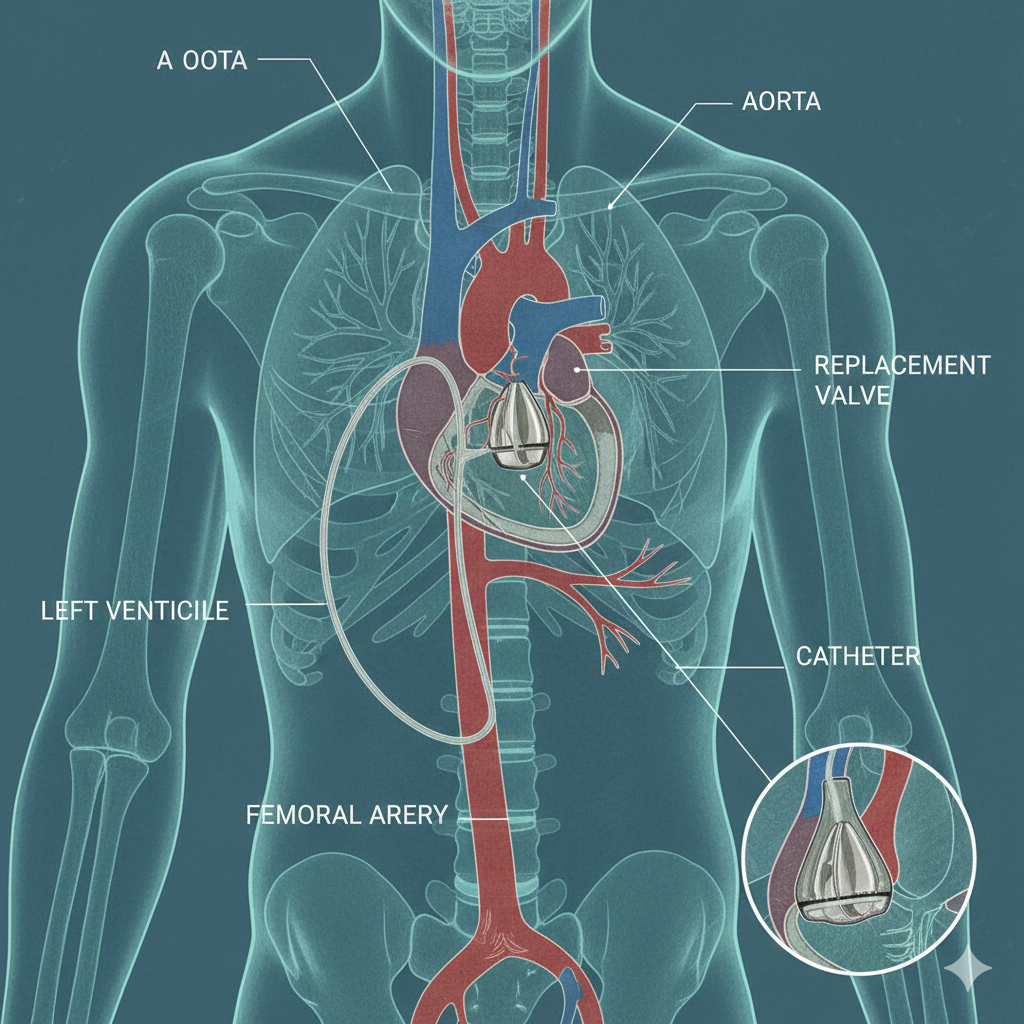
4.The Insemination
Approximately 36 hours after the trigger shot, the IUI procedure is performed quickly and painlessly. The physician gently passes a thin, flexible catheter through the cervix and directly into the uterine cavity. The prepared, concentrated sperm sample is slowly deposited high in the uterus.
5.Post-Procedure Care and The Two-Week Wait
Following the procedure, the woman can resume normal activities immediately. Your specialist may prescribe progesterone supplementation to support a potential pregnancy. The two weeks following the IUI are known as the “two-week wait” before a blood pregnancy test can confirm if the procedure was successful.
Success Rates and Considerations: Planning Your Next Steps
IUI Success Factors
IUI is less invasive and less expensive than In Vitro Fertilization (IVF), making it a highly desirable intermediate step. However, understanding the factors influencing success is vital for planning your journey:
- Age is the Primary Factor: For women under 35, success rates per cycle generally range from 15% to 20%. For women over 40, these rates drop substantially (often below 5%).
- Diagnosis Matters: IUI is most effective for cervical factor infertility and single women using donor sperm, and less effective for severe male factor issues.
- The Plateau Effect: Most pregnancies resulting from IUI occur within the first three to four cycles. If pregnancy does not occur after several well-timed IUI cycles, your fertility specialist will typically recommend considering IVF.
Looking Ahead: A Continuum of Care
The journey through fertility treatments is deeply personal, and the right plan is one that evolves with your needs and response to therapy. At Blossom Women’s Clinic, we stand ready to guide you through every step, beginning with the simplicity of ovulation monitoring and moving seamlessly to targeted treatments like IUI. We also provide a full suite of advanced reproductive technologies, including In Vitro Fertilization (IVF) and fertility preservation, ensuring that whatever your next step may be, you have a caring and expert team beside you.
Take the First Step Towards Parenthood
Understanding your body and the available treatment options is the most powerful tool you have. If you are ready to move from trying to planning, we invite you to schedule a comprehensive fertility consultation with our specialists. We are committed to offering compassionate, evidence-based care tailored to your unique journey.