Stressed and Struggling? How Stress Impacts Your Reproductive Health
Stress isn’t just an emotion — it’s a biological signal. Learn how chronic stress affects menstrual cycles, fertility, libido, and long-term reproductive health, and discover practical, stage-specific strategies from Blossom Women’s Clinic.

The body keeps the score: stress, hormones and the HPG axis
We live in a fast-paced world where juggling work, relationships and family responsibilities can feel relentless. That chronic activation shows up physiologically — especially in the Hypothalamic–Pituitary–Gonadal (HPG) axis, the key regulator of reproductive hormones. At Blossom Women’s Clinic, we treat stress as both a symptom and a modifiable driver of reproductive health concerns.
How it works
When stressed, the brain increases cortisol and adrenaline. Short bursts of these hormones help us respond to immediate threats. But when cortisol stays high, it dampens the hypothalamus’s release of GnRH (the hormone that kickstarts the reproductive cascade). This interferes with ovulation, menstrual regularity, and even libido. Men are affected, too — chronic stress can negatively influence sperm concentration, motility and DNA integrity.
Quick facts
- High cortisol can lead to functional hypothalamic amenorrhea (missed cycles without a structural cause).
- Stress worsens PMS/PMDD by changing neurotransmitter balance (serotonin, GABA).
- Inflammation and the gut microbiome are important mediators between stress and hormonal health.
Common ways stress shows up in your reproductive health
- Missed or irregular periods: cycles that are shorter, longer or absent.
- Anovulation: ovulatory cycles without egg release, reducing natural fertility.
- Worsened menstrual symptoms: heavier cramps, mood swings, and fatigue.
- Low libido and relationship strain: emotional burnout often lowers sexual desire.
- Challenges during fertility treatment: higher stress can impact treatment tolerance and mental wellbeing during IVF or IUI.
Myth vs. Fact
Myth
Myth: “Stress alone can permanently make you infertile.”
Fact
Fact: Stress can temporarily disrupt cycles and ovulation, but effects are often reversible with targeted care — including lifestyle changes, medical evaluation, and support. Permanent infertility is uncommon and usually linked to other medical causes.
Did you know?
- Even short-term stressors (like major exams or travel) can delay ovulation by a cycle or two.
- Supportive relationships and talk therapy have measurable benefits on cortisol levels and overall fertility outcomes.
- Men with high chronic stress have been shown to produce sperm with lower motility and higher markers of oxidative stress.
Checklist: Practical steps you can start today
- Track your cycle for at least 3 months (apps or paper). Note stressors, sleep and diet.
- Aim for 7–9 hours of quality sleep with consistent bed/wake times.
- Add 10–20 minutes of daily mindfulness or breathing practice.
- Replace two high-caffeine drinks with herbal tea or water each day.
- Schedule a weekly restorative activity (walk, hobby, spending time with loved ones).
- If trying to conceive: share your concerns with your fertility clinician — a small adjustment can make a big difference.
How Blossom Women’s Clinic supports you
We take a person-first approach: medical assessment, lifestyle support and emotional care. Our team coordinates tests and treatments while offering practical stress-management tools tailored to your life stage and goals.
- Comprehensive testing: hormonal panels, thyroid screening, and targeted labs.
- Personalized plans: nutrition, supplementation, gentle exercise plans, and sleep support.
- Mind-body support: referrals for CBT, mindfulness training, and specialist counseling during fertility care.
How stress affects different life stages
Teens & young adults
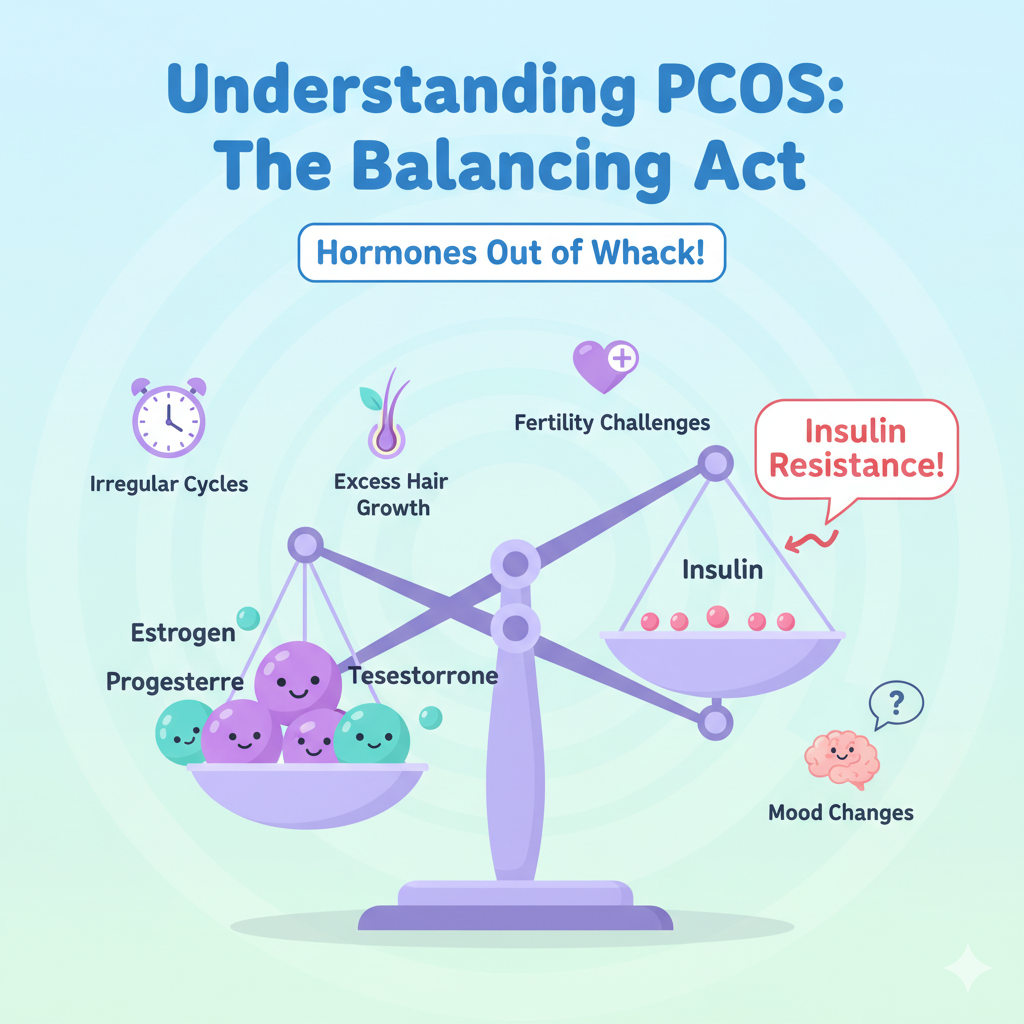
Adolescence is a sensitive time: hormonal changes combine with academic and social pressures. Irregular cycles are common, but if missed periods, severe pain or mood changes occur, early evaluation helps rule out PCOS, thyroid issues, or functional hypothalamic amenorrhea.
- Encourage healthy sleep and balanced meals to support normal hormone maturation.
- Promote body-positive messages and reduce performance pressure where possible.
Pregnancy & trying to conceive
Stress does not prevent pregnancy in most cases, but chronic stress can interfere with ovulation and semen quality. During pregnancy, stress can affect sleep, appetite and blood pressure; robust support networks and stress mitigation strategies protect both parent and baby.
- Mindfulness and gentle prenatal yoga can reduce anxiety and promote better sleep.
- Discuss any history of anxiety or depression with your care team — early support improves outcomes.
Perimenopause & menopause
Midlife transitions bring hormonal shifts that interact with life stressors (career, caregiving). Sleep disruption, hot flashes and mood changes may feel worse with unmanaged stress. Treatment options range from targeted lifestyle changes to medical therapies for symptom relief.
- Prioritize sleep hygiene and consider cognitive-behavioral therapy for insomnia if needed.
- Discuss hormone therapy and non-hormonal options with your clinician for symptom control.
When to seek medical help
Seek evaluation if you experience any of the following:
- Absent periods for 3 months or more (if not pregnant or breastfeeding).
- Very heavy bleeding or severe pain that limits daily activity.
- Struggling to conceive after a year of trying (or 6 months if over age 35).
- Worsening anxiety or depression related to reproductive concerns.
Practical therapies and evidence-based tools
Here are modalities we commonly recommend alongside medical evaluation:
- Cognitive Behavioral Therapy (CBT) — effective for anxiety, insomnia and stress-related mood disorders.
- Mindfulness-based stress reduction (MBSR) — improves perceived stress and sleep quality.
- Nutritional support — targeted supplementation (iron, B12, vitamin D, omega-3) when indicated.
- Gentle exercise — prioritise consistency over intensity to avoid overtraining-induced hormonal suppression.