Understanding PCOS
Polycystic Ovary Syndrome (PCOS) is one of the most common hormonal disorders in women of reproductive age, affecting approximately 1 in 10 women worldwide. It’s a complex condition that involves an imbalance in reproductive hormones, which disrupts the normal functioning of the ovaries.
The name “polycystic ovary” refers to the appearance of the ovaries in many women with this condition – they may be enlarged and contain numerous small cysts (fluid-filled sacs) along the outer edge. However, it’s important to note that not all women with PCOS have cysts, and having ovarian cysts doesn’t necessarily mean you have PCOS.
1 IN 10
Women affected by PCOS
70%
50%
Women with PCOS develop diabetes
Did you know? PCOS is the most common cause of female infertility, but with proper management, many women with PCOS can successfully conceive and have healthy pregnancies.
Symptoms of PCOS

PCOS symptoms can vary widely from woman to woman and may change over time. Some women experience mild symptoms, while others have more severe manifestations. The most common symptoms include:
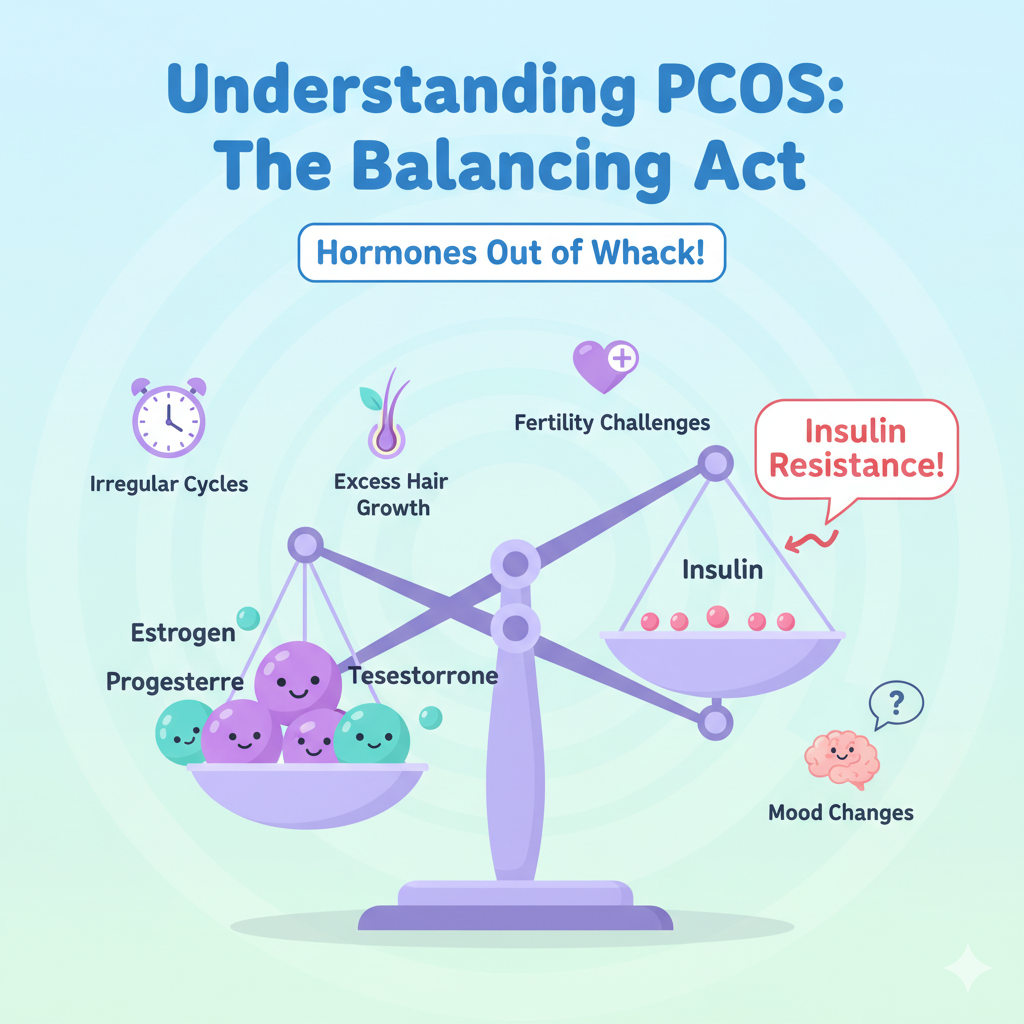
Irregular, infrequent, or absent menstrual periods
Excess hair growth on face, chest, or body
Severe acne and oily skin
Thinning hair or hair loss on the scalp
Weight gain, especially around the abdomen
Difficulty losing weight
Difficulty conceiving (infertility)
Darkening of skin in body folds
Skin tags in armpits or neck area
Mood changes, anxiety, or depression
Fatigue and low energy
Sleep problems or sleep apnea
Important: PCOS symptoms can be subtle and are often mistaken for other conditions, leading to delayed diagnosis. If you’re experiencing several of these symptoms, it’s important to consult with a healthcare provider.
Root Causes of PCOS

While the exact cause of PCOS isn’t fully understood, researchers believe several factors play a role in its development:
Hormonal Imbalance
Women with PCOS often have elevated levels of androgens (male hormones), which can prevent the ovaries from releasing eggs (ovulation) and lead to the development of cysts.
Insulin Resistance
Most women with PCOS have insulin resistance, meaning their cells don’t respond normally to insulin. This leads to higher insulin levels, which can increase androgen production and worsen PCOS symptoms.
Genetic Factors
PCOS tends to run in families, suggesting a genetic component. If your mother, sister, or aunt has PCOS, you may have a higher risk of developing it.
Inflammation
Chronic low-grade inflammation may contribute to PCOS by stimulating the ovaries to produce more androgens.
Research Insight: Recent studies suggest that PCOS may begin developing before birth due to exposure to high levels of androgens in the womb, which could program the body to develop PCOS later in life.
How PCOS Is Diagnosed

There’s no single test to diagnose PCOS. Instead, healthcare providers use a combination of approaches:
Medical History Assessment
Your doctor will ask about your menstrual cycle patterns, symptoms, and family history of PCOS or related conditions.
Physical Examination
This includes checking for signs of excess androgen (such as excess hair growth, acne, or male-pattern baldness) and measuring blood pressure, BMI, and waist size.
Blood Tests
These measure hormone levels including testosterone, LH (luteinizing hormone), FSH (follicle-stimulating hormone), and insulin. Thyroid function tests and cholesterol levels may also be checked.
Pelvic Ultrasound
This imaging test looks for cysts on the ovaries and checks the thickness of the uterine lining.
Most doctors use the Rotterdam criteria for diagnosis, which requires at least two of the following three features:
- Irregular or absent ovulation
- Clinical or biochemical signs of high androgen levels
- Polycystic ovaries on ultrasound
Early diagnosis benefit: Early diagnosis and treatment can help prevent long-term complications such as type 2 diabetes, heart disease, and endometrial cancer.
Complications of Untreated PCOS
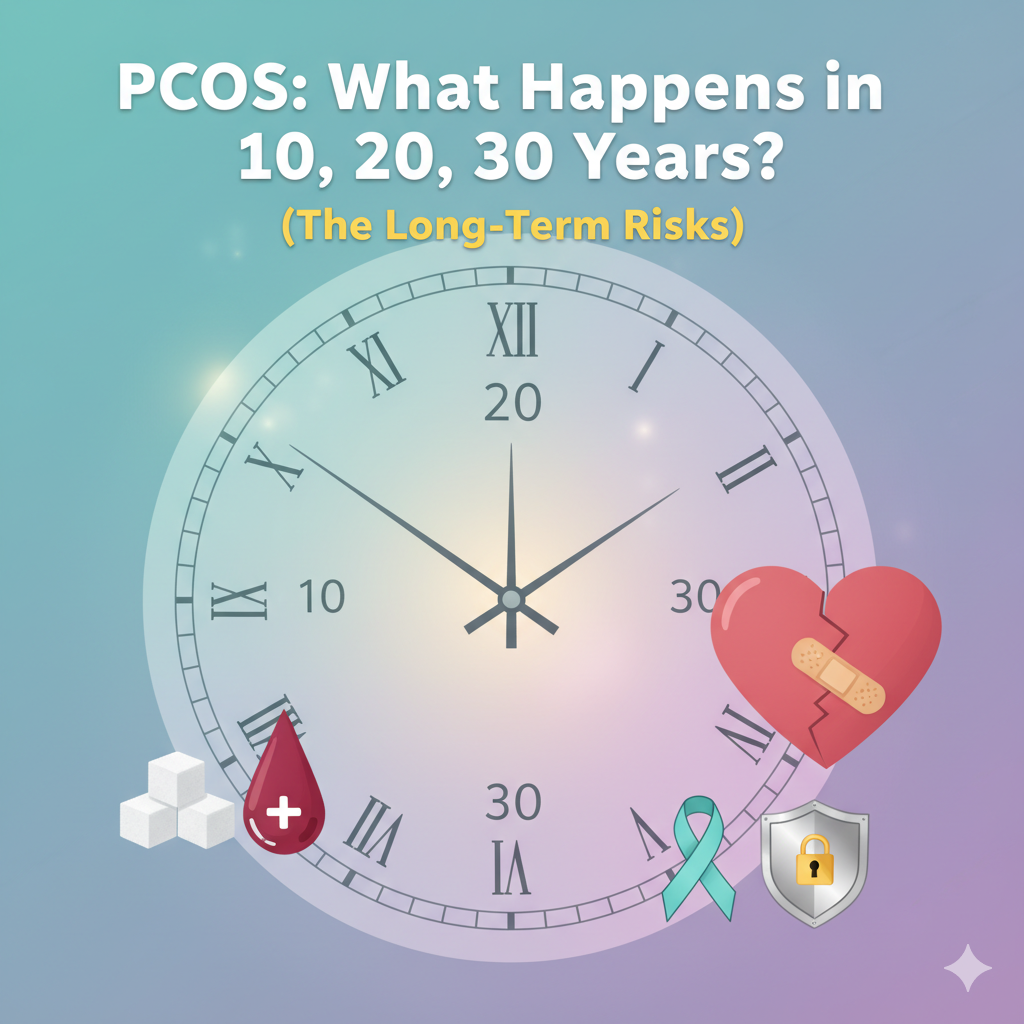
When left unmanaged, PCOS can lead to several serious health complications:
Metabolic Complications
- Type 2 Diabetes: Up to 50% of women with PCOS develop prediabetes or type 2 diabetes before age 40
- Metabolic Syndrome: A cluster of conditions including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels
- Cardiovascular Disease: Increased risk of heart attack and stroke
Reproductive Complications
- Infertility: Difficulty conceiving due to irregular ovulation
- Pregnancy Complications: Higher risk of gestational diabetes, preeclampsia, and premature birth
- Endometrial Cancer: Increased risk due to buildup of the uterine lining when periods are infrequent
Psychological Complications
- Depression and Anxiety: Higher rates of mood disorders among women with PCOS
- Eating Disorders: Increased risk due to body image concerns
- Poor Self-Esteem: Often related to physical symptoms like weight gain and excess hair
Other Complications
- Sleep Apnea: More common in women with PCOS, especially those who are overweight
- Non-Alcoholic Fatty Liver Disease: Inflammation and fat accumulation in the liver
Managing PCOS Effectively

Lifestyle Changes
A balanced diet and regular exercise are first-line treatments for PCOS:
- Choose complex carbs (whole grains, vegetables, legumes)
- Include lean proteins and healthy fats
- Aim for 150 minutes of moderate exercise weekly
- Even 5-10% weight loss can significantly improve symptoms
Medications
Various medications can help manage specific PCOS symptoms:
- Birth control pills to regulate periods
- Metformin to improve insulin sensitivity
- Fertility medications like clomiphene
- Anti-androgen medications for excess hair and acne
Complementary Approaches
Some women find these approaches helpful alongside conventional treatment:
- Inositol supplements to improve insulin sensitivity
- Acupuncture for menstrual regularity
- Mindfulness and stress reduction techniques
- Support groups for emotional wellbeing
Personalized care matters: Each PCOS case is unique and requires an individualized approach. What works for one woman may not work for another, so it’s important to work closely with your healthcare provider to find the right combination of treatments for you.
How Blossom Women's Clinic Helps

At Blossom Women’s Clinic, we specialize in comprehensive PCOS care with a focus on your individual needs and goals. Our multidisciplinary approach includes:
- Comprehensive Diagnostic Services: Advanced hormone testing, pelvic ultrasounds, and metabolic assessments
- Personalized Treatment Plans: Tailored combinations of lifestyle interventions, medications, and supplements
- Nutritional Counseling: PCOS-specific meal planning and dietary guidance from registered dietitians
- Fertility Support: Ovulation induction, timed intercourse guidance, and referral to reproductive specialists when needed
- Mental Health Services: Counseling and support for the emotional challenges of PCOS
- Long-Term Health Monitoring: Regular screenings for diabetes, cardiovascular risk, and other PCOS-related complications
Our mission is to empower women with PCOS to take control of their health and live their fullest lives. We believe in treating the whole person, not just the symptoms.


